Vous êtes au centre: Votre Expérience, Vos Résultats.
It's About You: Your Experience, Your Results.

Shockwave Therapy
PAIN RELIEF IN A FEW SESSIONSExtracorporeal shockwave therapy (ESWT) has been found to bring relief in most patients with muscluloskeletal pain after just a few treatment sessions, even in patients suffering from chronic pain. This non-invasive therapy activates a self-healing process where pain occurs and achieves significant results.
Myofascial trigger points (MFTPs) are a common cause of chronic neck and back pain. They are localized segments of muscle that are thought to be subjected to trauma by acute injury or microtrauma from repetitive stress. MFTPs can occur in any skeletal muscle. The diagnosis is clinical and includes the identification of small knots (2-5 mm in diameter) and tight bands within affected muscles that are painful when palpated. Diagnostic imaging is not helpful and should only be considered to rule out other causes of muscle pain.
It is still unclear whether or not MFTPs are true pathologic entities, however the resulting contraction of small parts of the muscle leads to diminished blood flow with subsequent ischemia and release of painful substances such as serotonin, histamine and prostaglandins in the affected area.
MFTPs are a very common condition, especially in the cervical musculature. Up to 85% of back pain and approximately 55% of neck pain and headaches are caused by myofascial pain.
The predominant age is 30 to 50 years. Women are more affected than men. Very often MFTPs are associated with poor posture. Notably MFTPs frequently produce neurological complaints including headache, dizziness, sensory symptoms, as well as gastrointestinal problems.
The treatment of MFTPs should start with a manual technique that involves applying pressure to a trigger point to release the pathologic contraction of the muscle segment and to stretch the segment to restore normal muscle fiber length. This can be accompanied by acupuncture, stress management and relaxation techniques. Pharmacologic treatment is unspecific and may comprise muscle relaxants, nonsteroidal anti-inflammatory drugs (NSAIDs), anticonvulsants, or topical application of local anesthetics or botulinum toxin.
Radial shock wave therapy (RSWT) is very effective for MFTPs and may mimic manual therapy in applying pressure to a trigger point to release the pathologic contraction of the muscle segment. Prevention of recurrence should focus on appropriate ergonomic changes in patients’ day-to-day activities to avoid repetitive stress to the injured muscles.

HOW IT WORKS
A shock wave is a single acoustic pulse characterised by a rapid rise to a high peak pressure followed by a rapid drop to below ambient pressure. They are sent to the affected area from the point of contact on the skin’s surface.
The Swiss DolorClast® Method uses single acoustic pressure waves to treat musculoskeletal and dermatological pathologies. It offers and combines two technologies – the propagation of radial and/or focused shock waves – to optimise treatment results.
SOME HISTORY
Originally developed for urology, pneumatically generated shock waves were successfully used on bone tissue as early as 1990.
Invented by EMS Electro Medical Systems, the Radial Shock Wave therapy was introduced in 1999 under the name “Swiss DolorClast® Method” and became the new standard in extracorporeal shock wave therapy.
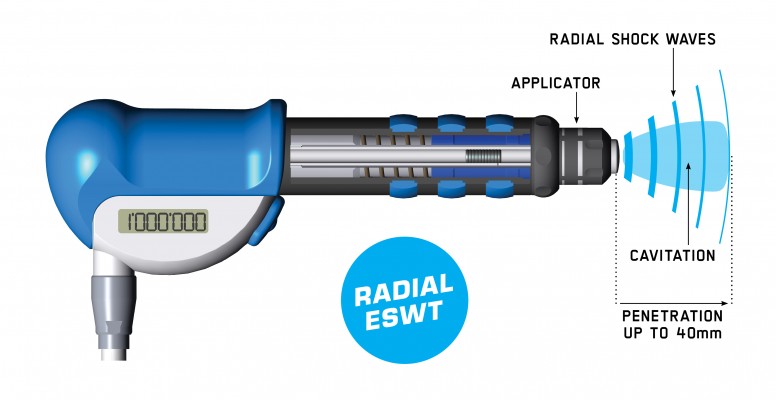
Ballistic Generation
Compressed air accelerates a projectile which strikes a fixed applicator.
The kinetic energy is converted into a shock wave delivered to the target tissue through the skin.
These shock waves are conveyed radially for broad treatment areas.
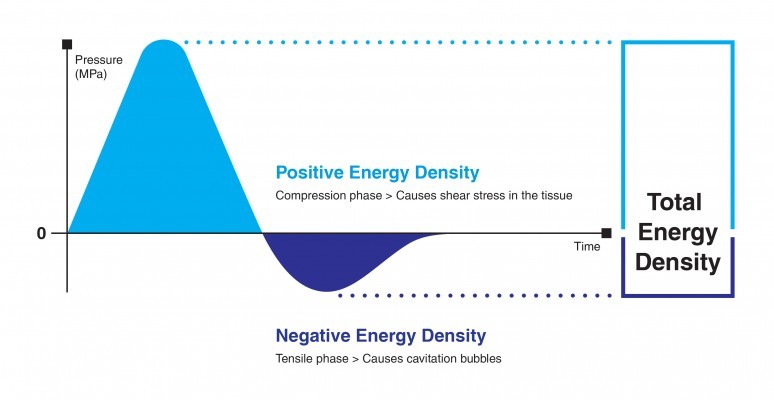
“A significant tissue effect is cavitation consequent to the negative phase of the wave propagation ” (Ogden et al., 2001)
“Both parameters (Compression phase and Cavitation) may have important consequences for therapeutic bioeffect ” (Perez et al., 2014)
“The contribution of cavitation to the therapeutic effect of radial shock waves was recently shown in an advanced animal model ” (Angstman et al., 2015)